Systematic Review of Low Pressure HBOT for Blast Induced Concussion & PTSD | A Clinical Case Study
Why do our nations service members return from deployment with PTSD?
This is a question we have been asking as doctors for years. Maybe, we have found a solution to the ever-growing problem.
Hyperbaric oxygen therapy or HBOT was studied in todays research review for treatment of blast induced concussion and post-traumatic stress disorder.
22 Veterans a Day
22 veterans a day commit suicide, and our nation’s best and brightest doctors have been struggling to understand how to combat this problem.
Drs. Harch and Amen have done extensive research into this problem and have accomplished a clinical study to measure the change in our veterans brains.
In this report they discuss the issues, their solutions and the results they achieved. Lets dive in, pun intended.
Safety and Efficacy of Mild HBOT
16 veterans who have been diagnosed with TBI or PTSD underwent a series of 40 dives lasting 60 minutes each at 1.5 ATM, a comparable level to what we use at Clarity.
They utilized symptoms, physical and neurological exams, spect brain imaging, neuropsychological and psychological testing to monitor change after the administration of HBOT was completed.
The effectiveness is as follows, directly from the article.
A Brief Article Snippet
“The remarkable findings in this study were the significant improvements in self-reported symptoms, physical exam changes, PCS symptoms, perceived quality of life questionnaires, affective measures (general anxiety, depression, suicidal ideation, and PTSD), cognitive measures (memory, working memory, attention, and FSIQ score), and SPECT brain blood flow imaging.
The magnitude of improvement was consistent across all domains measured. These findings were mirrored by a reciprocal reduction or elimination of psychoactive and narcotic prescription medication usage in 64% of those subjects for whom they were prescribed. Spontaneous improvement as an explanation for all of these findings is inconsistent with the natural history of PCS and PTSD 2.8 years after injury. Reduction in headaches and increase in FSIQ/cognitive function evidenced effectiveness of HBOT 1.5 ATA in the treatment of blast TBI/PCS cerebral wounds.
Headache Reduction
Headache is a marker of blast-induced PCS and distinguishes PCS from PTSD (Hoge et al., 2008). In our study 13/15 (87%) patients reported a substantial reduction in headaches during the 30 days they received HBOT. A reduction in headache and improvement in PCS symptoms (39% reduction in RPCSQ, p = 0.0002) is consistent with the treatment of the extracerebral marker of PCS, as well as the associated underlying biological injury caused by TBI. This biological wound is established in our subjects due to their loss of consciousness (Lidvall, 1975; Symonds, 1962). FSIQ increased 14.8 points to 110.6 ( p < 0.001). As a global measure of cognitive function this increase is consistent with the patients’ self-reported 40% cognitive improvement, the global nature of blast brain injury, and the global improvement in blood flow seen on SPECT.
IQ Increase
Some of the IQ increase could be explained by WASI FSIQ overestimation (Axelrod, 2002) compared to the WAIS-III, but the WASI has been validated in other adult heterogeneous clinical samples (Ryan, 2003; Hays, 2002). Our study was performed on a relatively homogenous patient group. The consistency of our findings despite different ways of measuring (WASI and PBNRS) argues against a significant contribution from a WASI flaw, and is consistent with the conclusion that the HBOT did improve overall cognitive functioning. Memory and frontal lobe function (simple sustained attention, working memory, and more complex attention) improved from what would appear to be ‘‘average’’ or ‘‘normal’’ levels to what the subjects considered to be more their ‘‘normal’’ levels.
Our results are very similar to cognitive improvements in a controlled chronic severe TBI HBOT study (Golden et al., 2006) and case report (Hardy, 2007). While only 26% of the subjects were TBI patients in the Golden study, 35 HBOTs in 35 days caused a significant 7.19-point increase in Stroop Color/Word score compared to normal and chronic brain injury controls, both of whom had similar 30- to 35-day test/retest intervals. The test/retest effect across 1- and 2- week intervals is 3.83 points (Franzen et al., 1987). The combined effect of Golden and test/retest (7.19 + 3.83 = 11.02) is nearly identical to the 11.0 point seen increase in our study.
Changes in Reaction Time
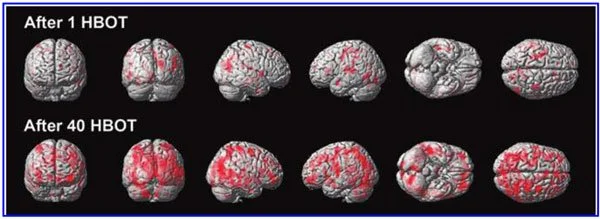
Changes in motor speed and fine motor coordination reached significance on only one of four measures, the Table 11. Top 10 Clusters of Voxels Showing Significant Increases in Brain Blood Flow Common to Brain Scans after 1 HBOT (p < 0.01 with FWE) and 40 HBOTs ( p < 0.001 with FWE) Increases in rCBF post-40 HBOTs masked by scan post-1 HBOT Coordinates Brain area Cluster size KE T XYZ 1. Occipital superior to temporal right 1581 38.78 22 - 78 28 2. Temporal superior left 514 33.8 - 56 - 12 4 3. Temporal right 360 31.84 52 - 32 - 20 4. Precentral left 917 29.4 - 44 - 2 40 5. Parietal superior right 11 26.2 34 - 52 60 6. Cuneus to occipital left 405 24.04 - 12 - 86 16 7. Cerebellum left 71 22.88 - 38 - 58 20 8. Cerebellum to lingual right 24 22.02 14 - 56 10 9. Post-central to supra-marginal right 203 21.51 36 - 32 68 10. Rolandic operculum right 85 21.11 60 - 18 12 FWE, family-wise error correction; HBOT, hyperbaric oxygen therapy; rCBF, regional cerebral blood flow. Fusion of significant single photon emission computed tomography (SPECT) clusters after 40 HBOTs masked by clusters after 1 HBOT with standard reference MRI T1 transverse image.
Numbers correspond to the top 10 significant clusters in Table 11 at the p < 0.001 level when masked inclusively by results after 1 scan at the p < 0.01 level, numerically ordered from highest to lowest T value. Significant clusters incidentally occurring on the same slices are also depicted. The color bar shows relative amplitude of rCBF improvement (rCBF, regional cerebral blood flow; HBOT, hyperbaric oxygen therapy; MRI, magnetic resonance imaging).
HYPERBARIC OXYGEN AND CHRONIC TRAUMATIC BRAIN INJURY 179 Grooved Pegboard for the dominant hand, while the P.I. recorded improvements of coordination in 90–100% of subjects who had abnormalities on baseline testing. Possible explanations for this discrepancy include: (1) testing of different sizes and groups of muscles (finger/hand for the psychometric tests versus the entire upper and lower extremities on physical exam); (2) investigator bias/non-blinding; (3) qualitative (physical exam) versus quantitative (psychometric) testing; (4) small number in the study.
The Rivermead Behavioral Memory (RBM) Paragraph Delayed Recall was the sole significant negative cognitive outcome. The RBM is only one subtest of a larger test, and was added because the test offered alternative forms of the paragraph for retesting purposes. The negative result may be a function of the limited range of the test, unequal difficulty of the different paragraphs, small number, problems with sustained attention immediately after our intensive HBOT schedule, or a true negative effect of HBOT on this component of memory.
SPECT Imaging Results
The SPECT findings were as impressive as the cognitive improvements, and were consistent with the bi-hemispheric increases in SPECT regional cortical blood flow reported by Neubauer and Golden (Golden et al., 2002). Both texture and SPM analyses showed consistent and significant improvements in blood flow after 1 and 40 HBOTs compared to baseline, no significant difference in blood flow between 1 and 40 HBOTs, yet considerable overlap of the areas with improved blood flow after 1 and 40 HBOTs.
SPM also revealed more widespread significant increases in blood flow after 40 versus 1 HBOT (more voxels and brain regions) compared to baseline, and compared to texture analysis which showed the opposite, fewer ROIs with significant increases in blood flow after 40 versus 1 HBOTs. This discrepancy was due to an increased variance in blood flow after 40 HBOTs versus 1 HBOT that is evident on the reversal of SD and CV improvements in primarily gray matter ROIs from 1 to 40 HBOTs (2/3 right and left hemisphere white matter ROIs maintained the improvement in SD and CV after 40 HBOTs that were seen after 1 HBOT).
Some of the increased variance might be explained by the timing of imaging (within 4 h after the first HBOT and 48 h after the 40th HBOT), and the intensive twice/day, 5 days/week HBOT schedule. This increased variance is not captured on SPM due to the different analytical and statistical methods. Significant improvements in SPECT occurred after both 1 and 40 HBOTs; however, by historical precedent and design symptoms, cognition, and QoL were only tested after 40 HBOTs.
The symptomatic, cognitive, and QoL improvements evolved over the course of the treatment and no subject claimed significant symptomatic improvement after the first HBOT session. The dichotomous findings of SPECT improvement after 1 and 40 HBOTs and neurological function only after 40 HBOTs, and the differential effect of 40 HBOTs on white versus gray matter SPECT texture analysis strongly suggest different physiological effects of 1 and 40 HBOTs on the injured brain at different points in the treatment process.
Furthermore, the differential effect of 40 HBOTs on white versus gray matter is consistent with a biological effect of repetitive HBOT 1.5 ATA on the primary injury site in mild to moderate TBI, the white matter (Kraus et al., 2007; Lipton et al., 2009). An unexpected finding was the confirmation of a reduction in PTSD that was symptomatically observed in our first published case of PCS/PTSD (Harch et al., 2009a). In the present study subjects achieved a 30% reduction in PTSD scores in a 30-day period.
A biological substrate for this HBOT effect is difficult to identify. Symptomatically, combat blastinduced PCS is inextricably interwoven with blast-induced PTSD. PCS and PTSD share some common biological pathways, processes, and anatomy in the brain (Kennedy et al., 2007). The hippocampus, in particular, is a pathological target in both PCS (Umile, 2002) and PTSD (Bremner, 2007; Wang, 2010; Woon and Hedges, 2008). HBOT treatment of hippocampal PCS injury may explain some of the observed effect on PTSD symptom reduction seen in our study. Explanatory mechanisms for the HBOT effects are numerous.
Neubauer and associates (Neubauer et al., 1990) demonstrated that increased brain blood flow after a single HBOT in chronic cerebral ischemia (the Neubauer effect) predicted subsequent neurological improvement with repetitive HBOT. Ischemia is a known pathological process in TBI (Gaetz, 2004). Focal ischemia causes a post-transcriptional metabolic/protein synthesis impairment to neurons, termed the ischemic freeze (Hossman, 1993).
Ischemia and HBOT
The first HBOT may override this ischemic freeze, consistent with Siddiqui’s demonstration of improved oxygen capacitance of non-CNS ischemic tissue (Siddiqui et al., 1997). The increase in blood flow on SPECT after 1 HBOT session in our study may reflect this reversal of impaired protein synthesis. Simultaneously, it may test vascular reserve capacity similarly to the Wada test (Vorstrup, 1988). FIG. 6. Fusion of significant single photon emission computed tomography (SPECT) hippocampal increases in rCBF with standard reference MRI T1 transverse, sagittal, and coronal slices after 1 HBOT (row A) and 40 HBOTs (row C; p < 0.001 with FWE; FWE, family-wise error correction; rCBF, regional cerebral blood flow; HBOT, hyperbaric oxygen therapy; MRI, magnetic resonance imaging. 180 HARCH ET AL.
The global improvements in brain blood flow after 1 HBOT in our subjects were associated with improved function after 40 HBOTs, thus supporting the Neubauer effect’s prediction of neurological improvement. SPM analysis demonstrated considerable overlap of the areas with improved blood flow after 1 HBOT with those after 40 HBOTs, indicating that the areas identified on SPECT by the Neubauer effect are likely those responsible for neurological improvement after 40 HBOTs.
We have demonstrated the Neubauer effect in severe chronic TBI patients (Harch and Neubauer, 1999, 2004a,2009b,2009c; Harch et al., 1994,1996a; Neubauer et al., 1994), along with a pattern shift on SPECT after the first HBOT. The pattern shift consists of normalization (a relative decrease in high and increase in low blood flow; Harch and Neubauer, 1999,2004b; Harch, et al., 1996a) that is captured by a reduction in SD and CV in this study.
The first HBOT would not be expected to improve function, however, likely due to the limited impact of a single HBOT on blast-induced degenerated white matter (Bauman et al., 2009). The increased blood flow on SPECT, variance in MCP change, and improved neurological function seen after 40 HBOT sessions suggests a set of mechanisms different from those that occur after 1 HBOT session.
We propose that these mechanisms are the typical trophic mechanisms of HBOT in chronic non-central nervous system wounds (Gesell, 2009). Repetitive HBOT stimulates angiogenesis in chronic non-CNS wounded tissue (Marx et al., 1990), most likely by genomic effects (Godman et al., 2009), and has been shown to increase blood vessel density in injured hippocampus in our chronic rat TBI model, where the progenitor of this HBOT protocol was tested (Harch et al., 2007).
HBOT-induced increased hippocampal blood vessel density in this model highly correlated with improved spatial learning and memory. In our subjects SPECT SPM analysis showed significant improvements in blood flow in the hippocampus, while our subjects achieved significant gains in memory. These blood flow and memory improvements seen in our subjects are consistent with a trophic effect of HBOT on chronic brain wounding in the hippocampus, and possible healing/reinnervation of denervated tissue (Bauman et al., 2009).
Other mechanisms may contribute to the HBOT effects seen in our study. A single hyperbaric oxygen reoxygenation session causes prolonged excitability and neural plasticity of hippocampal neurons after exposure to hypoxia (Garcia et al., 2010), consistent with the Neubauer effect generated in this study. Repetitive HBOT has shown increased neurogenesis and cerebral blood flow in chronic global ischemia (Zhang et al., 2010). Zhang and associates administered repetitive HBOT 30 days after ischemic insult, similar to the 50-day delay in our animal model (Harch et al., 2007).
Blood Vessel Growth (Angiogenesis)
Neurogenesis has been shown to occur in association with angiogenesis (Palmer et al., 2000). As mentioned above, angiogenesis is a known trophic mechanism of HBOT, and may be responsible for the increased blood vessel density seen in our animal model (Harch et al., 2007). HBOT has also been shown to cause the release of bone marrow stem cells into the peripheral circulation (Thom et al., 2006). Peripheral stem cells are known to cross the blood–brain barrier (Mezey et al., 2003). The limitations of the present study were a lack of confirmation of post-injury brain MRI results in some subjects, unblinded investigators (except for the SPECT brain imaging SPM analysis), and lack of a control group.
The lack of confirmation of brain MRI findings in a few subjects could confound study results only by inadvertent inclusion of non clinically-apparent neurological disease that was manifest on MRI alone. We believe this is a very remote possibility; these young men were highly fit pre-military, underwent regular fitness evaluations while in the military, and had no premorbid disqualifying conditions. All symptomatology commenced with the incident blast and was present continuously since the blast.
MRI Results
Routine late MRI evaluations in mild to moderate TBI are usually negative, consistent with the majority of the scans in our subjects. We presume the few missing data points would similarly be normal or non-contributory. Investigator bias and placebo effects possibly contributed to the magnitude of some of the effects we measured, but are unlikely to account for the majority of the effects or the consistency and magnitude of the effects seen across all domains, particularly SPECT. Investigator bias could be present in the P.I.’s symptom and physical exam recording, and in S.R.A.’s neuropsychological testing, but it does not explain the significant SPECT findings for which separate independent analyses, one of which was blinded, were performed by E.F.F. in North Dakota and D.A. and D.V.T. in California.
None of the SPECT co-investigators interacted with the subjects, and they performed their analyses months after the subjects had completed their final imaging. Importantly, the blinded SPECT analyst, D.V.T., produced the most significant statistical results. Placebo effects cannot be entirely ruled out; however, there are multiple arguments against this notion. Treatment effect size in two meta-analyses of randomized placebo-controlled trials versus observational studies performed on the same treatments has been shown to be very similar (Benson and Hartz, 2000; Concato et al., 2000). This suggests that placebo effects are overestimated in observational studies such as ours.
Placebo effects on many of the cognitive measures in our study have been reported to be smaller than the changes we found with HBOT for FSIQ and WMS Visual Immediate and Delayed Memory (Doraiswamy et al., 2007), for Stroop Reaction Time (Calabrese et al., 2008), and for Stroop Color/ Word raw score ( Jorge et al., 2010). The placebo effects reported on SPECT in psychiatric disease, in healthy individuals, and in neurological disease have shown focal changes in regional cerebral blood flow (Beauregard, 2009), most commonly in the inferior frontal gyrus, striatum, and rostral anterior cingulate cortex ( Jarcho et al., 2009).
The global diffuse changes we measured have not been reported. In addition, it is highly improbable that a placebo effect could account for the multiplicity of differential changes on SPECT seen after 1 and 40 HBOTs using two different forms of mathematical/ statistical analyses. Lastly, the parallel improvements in memory scores and hippocampal blood flow are inconsistent with a placebo effect. Test/retest practice effects could explain some of the cognitive improvements; however, practice effects do not fully explain our measured increases for seven reasons. (1) Practice effects on the WAIS-III FSIQ over a mean 34.6-day retest interval have been shown to be 2.0–3.2 points across all age groups, 6 points in the 16- to 29-year-old group, and decrease with age; our subjects averaged 30 years old (Tulsky and Zhu, 1997).
They have also been shown to increase 6 points over 3- or 6-month retest times (Basso et al., 2002). Six points is 41% of the measured FSIQ increase on the WAIS-IV in our subjects. HYPERBARIC OXYGEN AND CHRONIC TRAUMATIC BRAIN INJURY 181 (2) The bulk of practice effects occur on the first retest (Bartels et al., 2010; Falleti et al., 2006), and our subjects had been cognitively tested at least once before our pre-HBOT testing session. Second and third retest (third and fourth tests) effects should have been smaller than 6 points. (3) Working memory has been shown to be among the most resistant to practice/ retest effects (Bartels et al., 2010; Basso et al., 2002).
Our subjects averaged a 9.9-point statistically significant improvement. (4) Practice effects are usually studied in normal individuals with intact memory function. Intact memory is a prerequisite for learning/practice effects. In individuals with impaired memory function, such as our subjects, practice effects may be less (Basso et al., 2002). (5) We used the alternate form WASI for the post-treatment IQ test in order to minimize practice effects. (6) A Stroop Color/Word score increase in a controlled HBOT study of chronic brain injury produced results similar to ours (Golden et al., 2006). (7) Stroop Color/ Word test/retest effects across 1- and 2-week intervals are 3.83 points (Franzen et al., 1987), and our increase was 11.0 points.
Limitations of 40 Sessions
Our results were achieved with half (40 HBOTs) of our normal protocol (80 HBOTs) on an accelerated twice/day schedule due to time and fiscal constraints. Through clinical experience, clinical research, and an animal pilot study that compared sham HBOT, 40, and 80 HBOTs (Harch et al., 1996b), we found greater cognitive and blood flow improvements (in an animal model; Harch et al., 2007), and clinical and blood flow improvements (in human cases) with 80 HBOTs, but the cases were primarily chronic moderate to severe TBI (vide supra). Neubauer and Golden (Golden et al., 2002) reported progressively greater blood flow in a case series of chronic severe brain-injured patients receiving 70 low pressure HBOTs. Recently, Wright and colleagues (2010) reported the effectiveness of our HBOT 1.5 ATA protocol in two airmen with blast-induced PCS, using 40 and 80 HBOTs (for persistent symptoms after 40 HBOTs).
Our subjects finished HBOT with partial improvement in their symptoms. It is likely that additional HBOT sessions would be beneficial.
Article Conclusion
In conclusion, application of a lower-pressure protocol of 40 HBOTs at 1.5 ATA to a 16-subject cohort of military subjects with blast-induced chronic PCS and PTSD was found to be safe. One fourth of the subjects experienced transient clinical deterioration halfway through the protocol and one subject did not finish. Simultaneously, as a group the 15 subjects experienced notable improvements in symptoms, abnormal physical exam findings, cognitive testing, PCS and PTSD symptom questionnaires, quality-of life questionnaires, depression and anxiety indices, and SPECT brain blood flow imaging that are inconsistent with the natural history of PCS 2.8 years post-injury.
The symptomatic improvements were present at 6-month phone follow-up in 92% of subjects who reported improvement after 40 HBOTs. More objective psychometric testing and SPECT imaging were not performed to confirm the durability of the HBOT treatment effect.
Sixty-four percent of the patients on psychoactive and narcotic prescription medications were able to decrease or eliminate use of these medications.
These data are preliminary and need confirmation with larger numbers of subjects or with a stronger design such as a randomized or Bayesian study. Acknowledgments The authors thank The Marine Corps Law Enforcement Foundation, The Semper Fi Fund, The Coalition to Salute Americas Heroes, the Harch Hyperbaric Research Fund of the Baromedical Research Institute of New Orleans, Mr. Caleb Gates, New Orleans Natural Resource Group, Rubie and Bryan Bell, Martin and Margaret Hoffmann, John and Virginia Weinmann, Dr. Warren Thomas, Joan C. White, Health Freedom Foundation, Soldiers Angels, Operation Homefront Louisiana, The Audubon Society, Mr. Theodore Solomon, New Orleans Steamboat Company, the National WWII Museum, and Westwego Swamp Boat Tours for their generous donations. We thank Mr. Martin Hoffmann, ex-Secretary of the Army (President Gerald Ford) for his indefatigable fundraising efforts, Sean Bal and Ray Crowell, our hyperbaric technicians for their expert and safe delivery of hyperbaric oxygen therapy, Wanda Phillips for review of all of the study records, and Amy Trosclair of the BRI for overseeing the handling and disbursement of funds.
What This Means For You Or A Loved One
The results of this study are encouraging. It show clinical significant data to prove a decrease in symptoms associated with TBI and PTSD. There is always hope for those who seek it. Seek hyperbaric care at Clarity Hyperbarics in Des Moines or order your own chamber today!